ARFID and Autism
Avoidant/Restrictive Food Intake Disorder (ARFID) is a relatively new term introduced in 2013 with its inclusion in the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (1)
Previously known as Selective Eating Disorder, ARFID marks a distinct departure from its previous classification under a broader category of feeding disorders.
As a paediatric dietitian familiar with the challenges faced by families dealing with ARFID, I understand the seriousness of this condition and its impact on daily life.
Unlike mere picky eating, ARFID entails a pattern of eating that involves avoiding certain foods or food groups entirely and/or restricting food intake in terms of quantity, independent of available food or cultural norms.
It is important to note that ARFID is not driven by body image concerns, weight loss goals, or other behaviours typical of restrictive eating disorders like anorexia or bulimia.
In this blog, we’ll delve into the complexities of ARFID and its relationship with autism spectrum disorder, shedding light on the unique challenges faced by individuals and families navigating these conditions.

What is ARFID
Avoidant/Restrictive Food Intake Disorder (ARFID) is a complex eating disorder characterized by a persistent avoidance or restriction of food intake that leads to significant nutritional deficiencies, impaired growth, and/or significant interference with psychosocial functioning.
The diagnostic criteria for ARFID, as outlined in the DSM-5, include:
Diagnostic criteria for ARFID according to DSM V (2)
| A. An eating or feeding disorder (e.g., an apparent lack of interest in food or eating; avoidance of foods because of their sensory characteristics; concern about the consequence of eating), which manifests as an inability to get adequate nutrients and/or energy into the body with food and links to at least one of the following: 1. Significant weight loss (or lack of expected weight gain or growth in children); 2. Significant nutritional deficiencies; 3. Dependence on enteral feeding or oral food supplements; 4. Disturbances in psychosocial functioning. |
| B. The disorder cannot be explained by lack of food availability or cultural and religious reasons/practices. |
| C. This disorder does not occur exclusively in the course of anorexia nervosa or bulimia nervosa and is not the result of abnormalities in the experience of body weight and shape. |
| D. This disorder cannot be explained by the current state of health or other co-occurring mental disorders. |
Individuals with ARFID may exhibit a wide range of behaviours related to food intake, including extreme selectivity in food choices based on sensory characteristics (such as texture, taste, or smell), fear of aversive consequences associated with eating (such as choking or vomiting), or general disinterest in food (2).
In both the ICD-11 and DSM-5, the diagnostic criteria for Avoidant/Restrictive Food Intake Disorder (ARFID) emphasize the significant impact on an individual’s physical health and overall functioning.
ARFID is defined by avoidance or restriction of food intake, leading to inadequate energy or nutritional intake, which can result in weight loss, nutritional deficiencies, or reliance on supplements or tube feeding.
Additionally, ARFID can cause significant impairment in various aspects of life, including personal, family, social, and educational functioning, as well as stress related to social eating experiences.
This comprehensive definition underscores the severity and complexity of ARFID and highlights the importance of early recognition and intervention to mitigate its adverse effects on individuals’ well-being.
Prevalence of ARFID
While accurate prevalence rates for ARFID are challenging to determine due to underreporting and misdiagnosis, research suggests that it is more common in children and adolescents than previously recognized.
Recent studies indicate that ARFID may account for a significant portion of feeding-related concerns seen in paediatric healthcare settings, with estimates ranging from 5% to 14% to 22.5% in outpatient paediatric eating disorder treatment programmes (2). Studies have shown that it affects boys more than girls.
However, little is known about the rates of ARFID in adults in the general population (3). Recent studies show that it affects approximately 9.2% of adult patients with eating disorders. It affects women much more often than men [4,5)
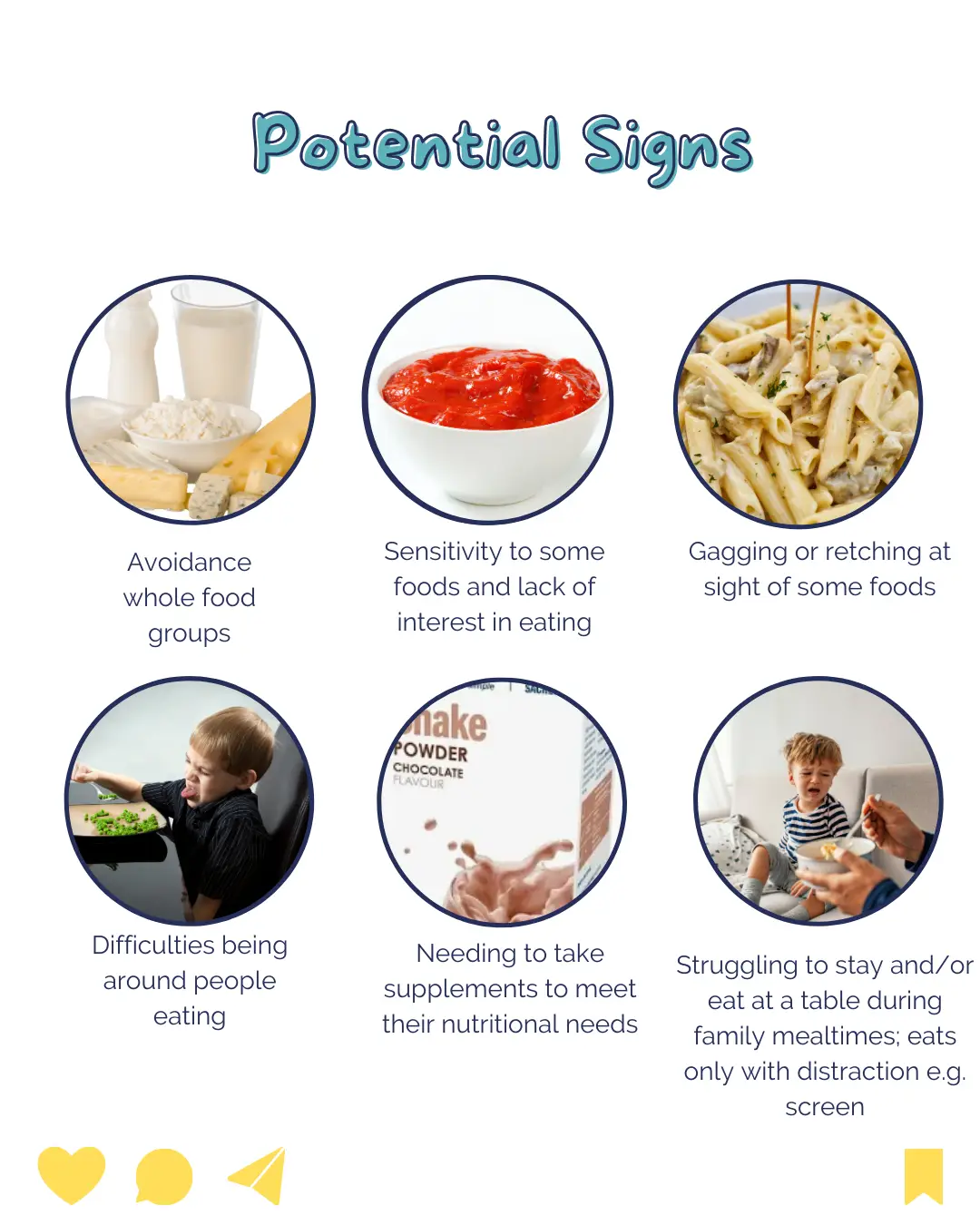
Signs and Symptoms of ARFID
Symptoms and behaviours associated with ARFID can vary widely among individuals but commonly include:
- Selective eating or avoidance of certain foods or food groups, often leading to a limited diet.
- Sensory sensitivities to food textures, tastes, smells, or appearances.
- Anxiety or fear related to eating, such as fear of choking or vomiting.
- Ritualistic eating behaviours or mealtime routines.
- Difficulty with transitions or changes in food presentation or environment.
- Physical symptoms of malnutrition or nutritional deficiencies, such as fatigue, weakness, or poor concentration.
- Impaired social functioning or avoidance of social situations involving food.
In some studies sensory sensitivity to food traits (63%) and/or lack of interest in food (51%) were the most common factors for food avoidance (2).
Understanding the criteria, prevalence, and symptoms of ARFID is essential for early recognition, diagnosis, and intervention to support individuals and families affected by this challenging eating disorder.
Consequences of ARFID
The consequences of Avoidant/Restrictive Food Intake Disorder (ARFID) extend beyond the avoidance or restriction of certain foods, potentially leading to significant micronutrient and macronutrient deficiencies.
This can result in a range of health issues and abnormal development, particularly critical during periods of intense growth and development in children.
Deficiencies in vitamins such as B1, B2, B12, C, and K, as well as minerals like zinc, potassium, and iron, are commonly observed in ARFID patients, alongside lower intakes of protein, fats, and carbohydrates.
These nutritional deficiencies can lead to severe medical consequences due to malnutrition, underscoring the importance of early assessment and intervention by healthcare professionals such as dietitian.
In addition to physical health consequences, ARFID can disrupt social interactions, work, and family life, leading to feelings of isolation and low self-esteem.
While diagnostic criteria help identify ARFID, raising awareness among both the public and professionals is crucial for early diagnosis and appropriate management, as understanding the challenges faced by individuals with ARFID is essential in devising effective treatment strategies (2).
What is Autism Spectrum Disorder (ASD)
Overview of Austism spectrum disorders: Definition and Diagnostic Criteria
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder characterized by persistent deficits in social communication and interaction, as well as restricted, repetitive patterns of behaviour, interests, or activities. The diagnostic criteria for ASD, as outlined in the DSM-5, include:
- Persistent deficits in social communication and social interaction across multiple contexts, manifested by difficulties in social-emotional reciprocity, nonverbal communication behaviours, and developing and maintaining relationships.
- Restricted, repetitive patterns of behaviour, interests, or activities, manifested by stereotyped or repetitive motor movements, insistence on sameness or routines, highly restricted interests, and hyper- or hypo-reactivity to sensory input.
- Symptoms must be present in the early developmental period, but they may not become fully manifest until social demands exceed limited capacities, or they may be masked by learned strategies in later life.
- Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning.
These disturbances are not better explained by intellectual disability or global developmental delay.
What are the main symptoms of autism?
Autistic Individuals may present with a wide range of features and challenges, including:
- Social difficulties: Difficulty understanding social cues, maintaining eye contact, and engaging in reciprocal conversation.
- Communication challenges: Delayed language development, echolalia (repetition of words or phrases), and difficulty using language for social purposes.
- Repetitive behaviours: Engaging in repetitive movements (e.g., hand-flapping, rocking), adherence to rigid routines, and intense focus on specific interests.
- Sensory sensitivities: Heightened sensitivity or hypo-responsiveness to sensory stimuli, such as light, sound, touch, taste, or smell.
- Executive function deficits: Challenges with planning, organization, flexibility, and problem-solving.
- Emotional regulation difficulties: Difficulty understanding and expressing emotions, leading to meltdowns or emotional outbursts in response to changes or sensory overload.
Why do autistic people struggle with eating?
Food-related challenges are common among individuals with ASD and are often influenced by sensory sensitivities.
Many individuals with ASD may experience heightened or diminished sensory responses to food textures, tastes, smells, or appearances, leading to selective eating habits or aversions to certain foods.
For example, a child with ASD may refuse to eat foods with certain textures, such as mushy or crunchy foods, due to sensory discomfort.
Understanding the interplay between food and sensory sensitivities in ASD is crucial for supporting individuals in developing healthy eating habits and addressing feeding-related concerns effectively.
By recognizing and accommodating sensory preferences and aversions, caregivers and healthcare professionals can promote positive mealtime experiences and overall well-being for individuals with ASD.
Is ARFID common with autism?
Shared Characteristics: Overlapping Symptoms and Behaviours
The intersection of Avoidant/Restrictive Food Intake Disorder (ARFID) and autism spectrum disorder (ASD) often presents with shared characteristics and overlapping symptoms. Both conditions can involve:
- Sensory sensitivities: Individuals with both ARFID and ASD may experience heightened or diminished responses to sensory stimuli, including food textures, tastes, smells, or appearances. These sensory sensitivities can contribute to selective eating habits, food aversions, or difficulties with certain food textures.
- Rigidity and inflexibility: Both ARFID and ASD are associated with rigid or inflexible behaviours and routines. Individuals may exhibit a strong preference for familiar foods or specific mealtime rituals and may resist changes in food presentation or environment.
- Anxiety and fear: Anxiety and fear related to food and eating are common features of both ARFID and ASD. Individuals may experience anxiety or distress when confronted with unfamiliar foods, new eating environments, or sensory stimuli associated with eating.
- Communication challenges: Difficulties with communication, particularly related to expressing food preferences, dislikes, or discomfort, can complicate feeding interactions for individuals with both ARFID and ASD.
Recognizing the shared characteristics and overlapping symptoms between ARFID and ASD is essential for understanding the complex relationship between these conditions and tailoring interventions to address the unique needs of affected individuals.
Arfid and autism treatments
Diagnosing and treating ARFID in the context of Autism Spectrum Disorder presents unique challenges due to the overlap of symptoms and complexities associated with both conditions.
Some challenges include:
Differential diagnosis: Distinguishing between feeding difficulties related to ARFID and those associated with ASD can be challenging due to overlapping symptoms and shared characteristics.
A comprehensive evaluation by a multidisciplinary team, including a paediatrician, psychologist, and dietitian, may be necessary to accurately diagnose and differentiate between these conditions.
Treatment planning: Developing effective treatment plans for individuals with ASD and co-occurring ARFID requires a multidisciplinary approach that addresses both the underlying factors contributing to feeding difficulties and the unique needs of the individual.
Strategies may include sensory-based interventions, behaviour modification techniques, and dietary modifications tailored to the individual’s preferences and sensory sensitivities.
Family involvement: Engaging caregivers and family members in the treatment process is essential for supporting individuals with ASD and ARFID.
Educating families about the relationship between ASD and feeding difficulties, providing guidance on effective feeding strategies, and offering ongoing support and resources can help empower families to navigate mealtime challenges successfully.
Despite these challenges, early recognition, comprehensive assessment, and targeted interventions can help individuals with ASD and co-occurring ARFID develop positive eating habits, improve nutritional intake, and enhance overall quality of life.
Treating ARFID and Arfid: Multidisciplinary Approach
A multidisciplinary approach involving collaboration between dietitians, therapists, doctors, and other healthcare professionals is essential for addressing the complex needs of individuals with autism and arfid.
Each member of the team brings unique expertise and perspectives to the table, allowing for comprehensive assessment, personalised treatment planning, and ongoing support for the individual and their family.
Role of Dietitians
Dietitians play a central role in assessing nutritional status, identifying dietary preferences and aversions, and developing individualised meal plans that accommodate sensory sensitivities and address nutritional deficiencies.
Therapists, including occupational therapists and speech-language pathologists, can provide support for sensory integration, feeding therapy, and communication skills development.
Physicians oversee medical management, address any underlying medical concerns, and collaborate with other team members to ensure holistic care.
Treatment Plans for ARFID and Autism
Effective treatment planning for individuals with ARFID and Autism involves tailoring interventions to address their specific needs, preferences, and challenges. Strategies may include:
- Sensory-based interventions: Incorporating sensory-based approaches, such as desensitization techniques, sensory play activities, and gradual exposure to new foods, can help individuals with ARFID and Autism develop tolerance to foods and textures.
- Behaviour modification techniques: Implementing behaviour modification techniques, such as visual supports, and structured mealtime routines
- Dietary modifications: Working with a dietitian to develop individualised meal plans that accommodate dietary preferences, address nutritional deficiencies, and provide adequate calories and nutrients is essential for supporting optimal growth and development.
- Family education and support: Providing education and support for caregivers and family members is crucial for empowering them to navigate mealtime challenges effectively and advocate for the individual’s dietary needs.
- Offering resources, guidance, and ongoing support can help families feel more confident and capable in supporting their loved one with ARFID and Autism.
Practical Tips for Parents and Caregivers
Creating a Supportive Mealtime Environment
Establishing a supportive mealtime environment is crucial for promoting positive eating experiences and addressing feeding difficulties in individuals with Avoidant/Restrictive Food Intake Disorder (ARFID) and autism spectrum disorder (ASD).
Here are some tips for creating a supportive mealtime environment:
- Set a predictable routine: Establish regular meal and snack times to provide structure and predictability. Consistent mealtime routines can help reduce anxiety and resistance around eating.
- Create a calm atmosphere: Minimize distractions and sensory stimuli during meals to create a calm and eating environment. Reduce noise and provide comfortable seating to support attentive eating.
- Offer choices: Empower individuals with ARFID and ASD by offering choices based on their sensory preferences and preferred foods
Introducing New Foods
Introducing new foods to individuals with ARFID and ASD requires patience, persistence, and sensitivity to their unique needs and preferences.
Here are some strategies for gradually exposing individuals to new foods and desensitizing them to sensory challenges:
- Start small: Begin by introducing tiny amounts of new foods on a separate plate alongside familiar foods to reduce anxiety and resistance.
- Use gradual exposure: Gradually increase exposure to new foods over time, starting with foods that are similar in taste, texture, or appearance to familiar favourites. Encourage individuals to explore new foods at their own pace, without pressure.
- Incorporate sensory play: Engage individuals in sensory play activities involving food to desensitize them to different textures, tastes, and smells. Encourage hands-on exploration, such as touching, smelling, and tasting foods but go at the child’s pace

Further Research and Advocacy
While significant progress has been made in understanding and addressing ARFID and Autism, there is still much to learn and accomplish.
Further research is needed to explain the underlying mechanisms contributing to feeding difficulties in individuals with ASD and ARFID and to develop more effective interventions and support strategies.
Despite the challenges posed by ARFID and Autism, there is reason for hope and optimism. There are some great charities such as ARFID awareness UK and BEAT eating disorders.
By fostering a supportive and understanding environment, empowering individuals to explore and experiment with new foods, and providing ongoing support and encouragement, we can promote hope and empowerment for individuals with ARFID and Autism.
If you like any dietetic support with ARFID feel free to reach out with any questions.
Written by Emma Shafqat BSc RD, Dietitian and Nutritionist.
“Dietitian with a Difference” holds no liability for any adverse reactions that may arise from the advice in the blog. The content provided is for informational purposes only and does not replace professional medical advice.



